Age-related Macular Degeneration
By Dr. Domenic Turco Macular degeneration is an umbrella term for diseases that affect the macula—the location in the...
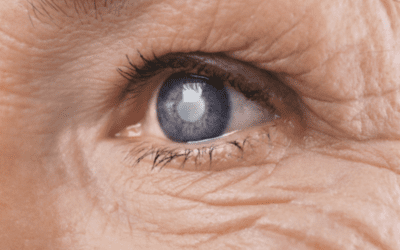
The Truth About Cataracts
By Dr. Jay Fiore A main fallacy with cataracts is that it “has to be ripe” before it can be removed. While it is true...
Shingles and Your Eyes
Shingles is a common viral infection that often appears as a painful, burning, or itchy rash. About one in three...
Dry Eye
By Dr. Jill Finke, OD Our eyes need moisture to be able to function well. Normally, a healthy tear film covers the eye...
Glaucoma
By Dr. Domenic Turco What is glaucoma? Glaucoma is an umbrella term for the eye disease that causes progressive damage...
Premium/Lifestyle Lenses
By Dr. Jeffery Heimer Advanced technology lens implants have been available to eye surgeons and their patients for...
Facts About Cataracts
By Dr. Jay Fiore A cataract is a clouding of the crystalline lens of the eye and a reversible cause of blindness. The...
Spring has Sprung
By Dr. Molly Wood Spring has sprung, and with that brings warmer weather, beautiful cherry blossoms and flowers in...
Signs or risk factors for eye disease
Both long- and short-term exposure to UV radiation can harm the eyes, affect vision to compromise overall eye health....