By Dr. Domenic Turco
What is glaucoma?
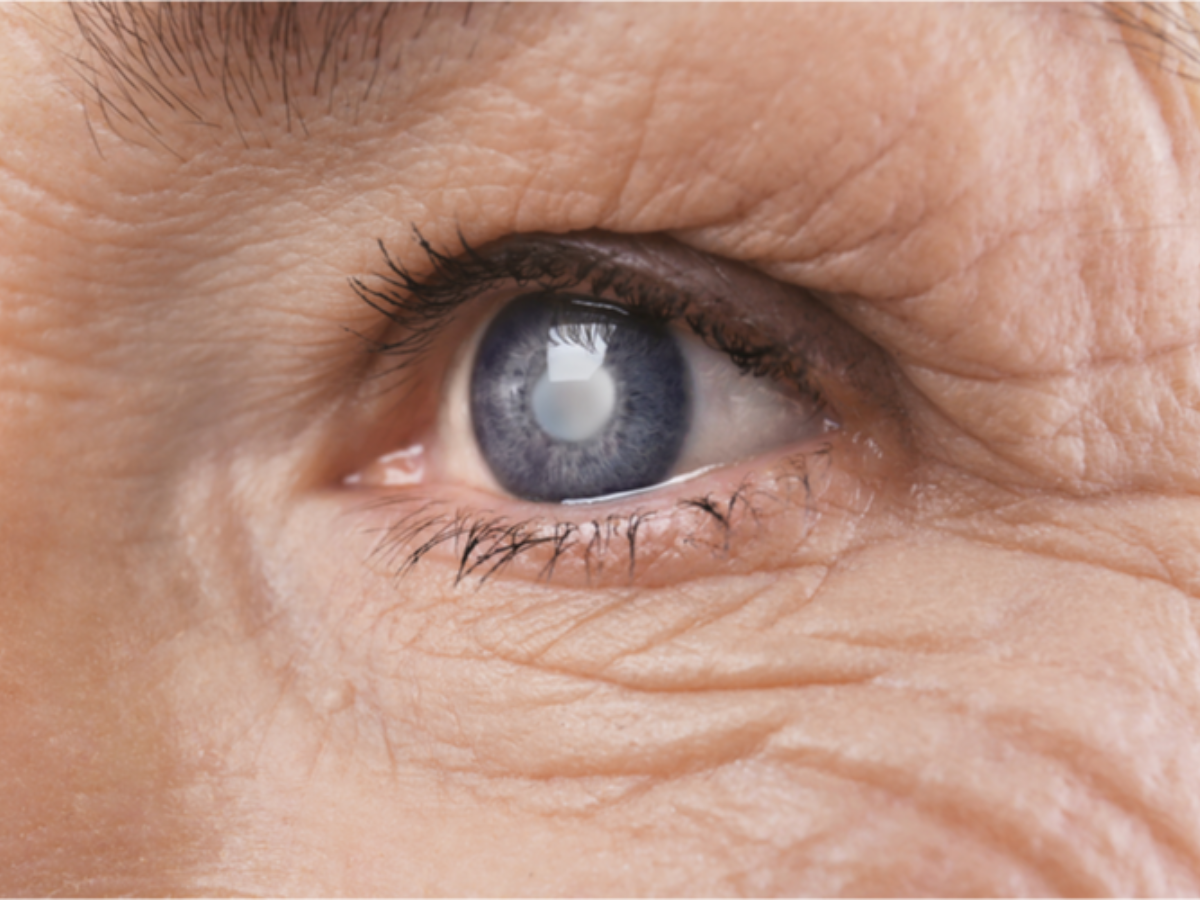
Glaucoma is an umbrella term for the eye disease that causes progressive damage to the optic nerve over time. There are different sub-categories of glaucoma such as open angle, closed angle, primary, and secondary, but they all demonstrate some form of optic nerve damage which can cause changes to both the appearance of the nerve as well as its function. The term “primary” means that the patient has no known eye disease or systemic disease causing the damage, while the term “secondary” implies the opposite. “Open” vs “closed” angle has to do with the anatomical structure of the angle of the eye, which is the location where fluid is drained from the front of the eye. It is important to make these distinctions as different types of glaucoma are treated differently. The most common type of glaucoma we encounter is primary open angle glaucoma (POAG).
What causes POAG?
The current understanding of POAG is that the fluid (aqueous humor) produced in the front part of the eye has increased resistance to drainage at the angle of the eye, which in turn causes a rise in the intraocular pressure. There is a common misconception that one has to have an elevated intraocular pressure to have glaucoma. Although we generally say that “normal” intraocular pressure is somewhere between 10-21 mm Hg, that is somewhat misleading as there are patients who demonstrate optic nerve damage and visual field changes despite having intraocular pressure in the so-called “normal” range. What this means is that there are other factors at play which we do not yet fully understand, including hereditary/genetic and possibly nutritional/environmental influences. Intraocular pressure is important because it is one of the few risk factors for glaucoma that we can modify with medication, lasers, and surgery.
How do you test for POAG?
When you see your ophthalmologist or optometrist for a glaucoma evaluation, you will likely undergo multiple tests to help make the determination of whether or not you have glaucoma. These include measurements of visual acuity, intraocular pressure, and central corneal thickness. Central corneal thickness is important as thinner corneas have been identified as a risk factor for glaucoma development. Your doctor may also perform gonioscopy, which utilizes a special mirrored lens to look at the anatomy of the angle of the eye. In addition to a slit lamp examination of your optic nerves, your doctor may also use an imaging modality such as optical coherence tomography (OCT) to look for areas of thinning of the nerve fiber layer surrounding the optic nerve. Changes in the nerve appearance or increasing thinning of the nerve fiber layer can be signs of progressive damage to the nerve. Finally, an assessment of your peripheral vision will be performed which is usually referred to as a visual field exam. This test is very important as glaucoma generally tends to affect peripheral vision before if affects central vision.
How do you treat POAG?
Once the diagnosis of glaucoma is made, your doctor will decide on a treatment that will best suit your needs as well as your personal preferences. As was mentioned earlier, intraocular pressure is one of the few risk factors that can be modified. The vast majority of POAG is treated by instillation of topical eye drops to lower the intraocular pressure by decreasing fluid production or increasing fluid outflow. There are multiple classes of medications designed to do this, and they include prostaglandin analogs, beta blockers, alpha agonists, and carbonic anhydrase inhibitors. Each class has its own unique side effect profile, and your doctor should discuss the risks and benefits of each medication before starting treatment. The most common initial topical therapy is the prostaglandin analog class secondary to ease of dosing, the fact that they are generally well-tolerated, and are effective in pressure lowering. Some patients will require more than one topical medication for control of their pressure.
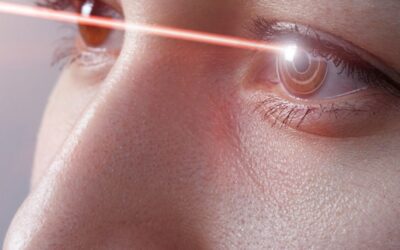
For patients whose pressure cannot be adequately controlled with topical medications or are intolerant of the side effects, there are the options of laser procedures and surgical procedures. Two of the most common types of lasers include argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT). Both lasers are generally well-tolerated and can be performed in the office setting. The surgical options for glaucoma have been expanding in recent years, ranging from the traditional trabeculectomy to less invasive procedures commonly referred to as MIGS (minimally invasive glaucoma surgery). It is beyond the scope of this article to go into all of the surgical options in detail, but they generally involve creating a pathway for fluid to drain from the eye and therefore lower the intraocular pressure. Any surgical discussion should include the risks and benefits of each procedure option.


0 Comments